Apartheid in medicine is not just a chapter in the past; it persists today, affecting countless communities. I urge you to look closely at the systemic inequalities that continue to undermine healthcare access for marginalized groups. Your understanding of these ongoing issues is vital for fostering change and promoting equity. By engaging with resources like the ALiEM Book Club: Medical Apartheid, you can gain insights into the profound impacts of these injustices.
Key Takeaways:
- Systemic racism in healthcare continues to result in unequal treatment and outcomes for marginalized groups.
- Historical abuses in medical research and practice have lingering effects on trust and access to care for communities of color.
- Awareness and advocacy are important to address ongoing disparities and ensure equitable healthcare for all populations.
Unequal Access: The Modern-Day Divide in Healthcare
Access to healthcare in the United States is plagued by profound inequalities, often dictated by socioeconomic status and location. Many marginalized communities face hurdles that result in higher rates of illness and death, reflecting a healthcare system that prioritizes profit over people. Disparities in insurance coverage, treatment options, and preventive care amplify the existing gaps, reinforcing the cycle of poverty and health inequity.
Socioeconomic Barriers to Treatment
Low income limits access to necessary healthcare services, forcing many to choose between basic needs and medical treatment. In some cases, a mere 20% of low-income individuals can afford out-of-pocket expenses, leading to delayed or entirely foregone care. Patients with low socioeconomic status often face a lack of transportation options and rigid work schedules, further exacerbating their inability to seek timely medical intervention.
Geographic Disparities in Medical Resources
Healthcare resources are not uniformly distributed, leading to stark geographic disparities. Rural areas often lack crucial medical facilities; approximately 80 million people live in regions classified as health professional shortage areas. Urban centers may have an abundance of healthcare providers, yet they can be inaccessible to those without reliable transportation or sufficient insurance coverage.
In rural America, almost 80% of counties are designated as primary care shortage areas, forcing residents to travel long distances for care. For instance, a patient in a remote part of Nebraska may have to drive over 60 miles to reach their nearest hospital, often lacking basic emergency services along the way. This lack of proximity to care leads to increased health complications, as conditions that could be managed with early intervention spiral into emergencies. Urban patients are not exempt from this issue; marginalized communities in cities often experience a shortage of quality care and health professionals willing to work in their neighborhoods, illustrating how geography can dictate your health outcomes.
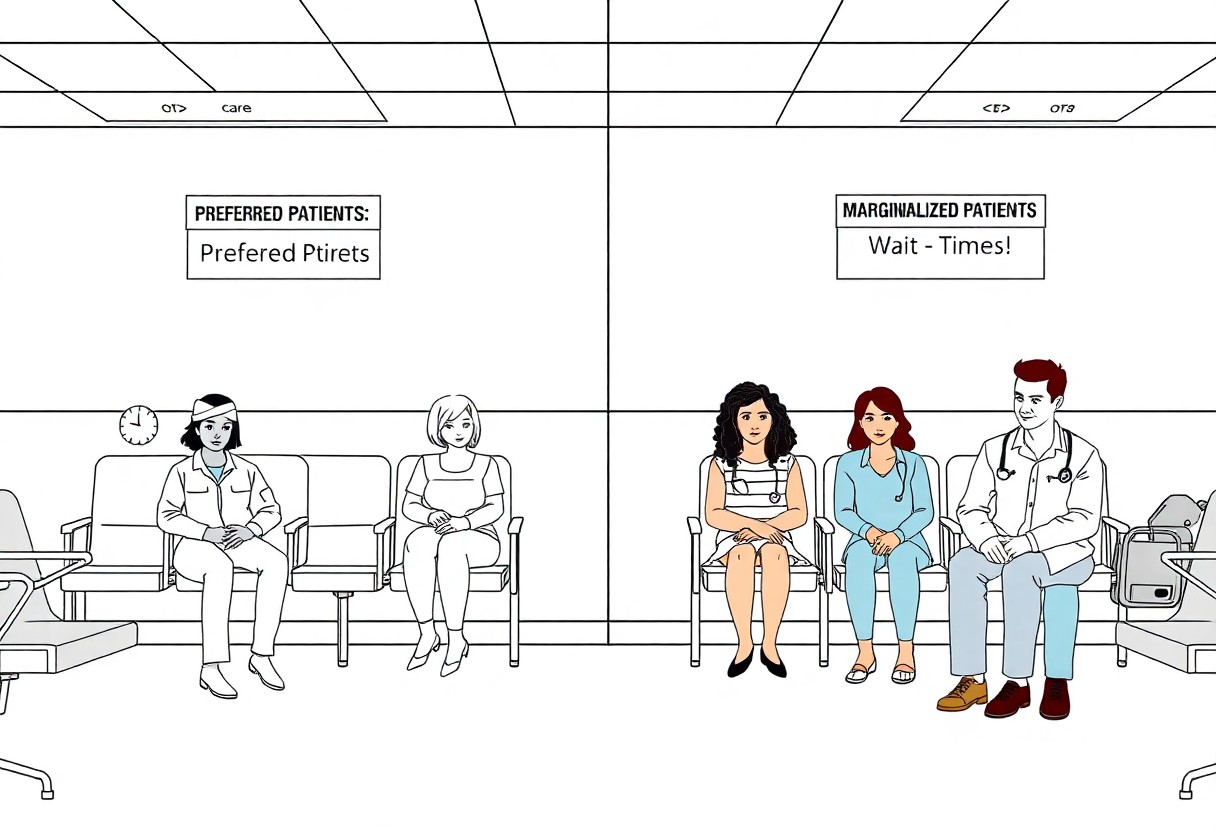
Racial Discrimination in Medical Practices
Racial discrimination manifests not only through overt actions but also through systemic policies that marginalize communities of color within healthcare systems. The struggles of patients accessing quality care continue, as reports reveal that Black patients are often undertreated for pain compared to their white counterparts. Medical Apartheid highlights these injustices and the necessity for reflection and reform in medical practices, reminding us that the echoes of past abuses still shape present circumstances.
Implicit Bias Among Healthcare Professionals
Implicit bias among healthcare professionals significantly influences treatment decisions, often resulting in disparities in the quality of care provided. Studies show that many practitioners harbor unconscious stereotypes that affect their interactions with patients, leading to less favorable outcomes for individuals from marginalized racial groups. This pervasive bias not only compromises patient care but also perpetuates longstanding inequities in the healthcare system.
The Impact of Historical Trauma on Patient Trust
Historical trauma plays a vital role in shaping the trust patients have in the healthcare system, particularly within marginalized communities. Many individuals carry the weight of past medical injustices, such as unethical experiments and neglect, which contribute to a deep-seated skepticism towards contemporary health practices. This distrust often results in delayed treatment and reluctance to engage with medical providers, creating a cycle that exacerbates health disparities.
In communities with histories of exploitation, the lasting effects of trauma are palpable. You may find that patients are less likely to seek preventive care or adhere to treatment plans due to fear of repeating past injustices. The Tuskegee Study and other infamous cases still resonate, leading to a pervasive atmosphere of mistrust towards healthcare institutions. Bridging this gap requires not only acknowledgment but a concerted effort from healthcare providers to foster a safe and welcoming environment for all patients.
The Role of Public Health Policies in Perpetuating Inequality
Public health policies often reflect and reinforce existing inequities, illustrating how Medical Apartheid remains relevant today. Policies that fail to consider the needs of marginalized populations can exacerbate disparities in healthcare access, funding, and quality. For every initiative designed to improve public health, there are others that inadvertently perpetuate systemic biases, leaving the most vulnerable communities without the support they desperately need.
Examining Legislation and Its Effects on Minority Communities
Legislation often neglects the unique challenges faced by minority communities, leading to continued disparities in health outcomes. For instance, policies that focus primarily on socioeconomic status without addressing the intersection of race can leave marginalized groups doubly disadvantaged. In these scenarios, you will find that reforms lack the necessary specificity, ultimately perpetuating cycles of inequality.
The Influence of Pharmaceutical Companies on Treatment Access
Pharmaceutical companies play a significant role in determining treatment accessibility for minority groups. The prioritization of profit over public health often results in exorbitant drug prices, disproportionately affecting those without adequate insurance or financial resources. Consequently, minority communities frequently face barriers to necessary medications and innovative treatments. This systemic issue underscores the need for transparent pricing and equitable distribution strategies.
The excessive influence of pharmaceutical companies extends beyond pricing; marketing strategies often target affluent demographics, ignoring the needs of underserved populations. As a result, healthcare providers may be less likely to prescribe medications necessary for treating conditions prevalent in minority communities. This inequity creates a stark reality where necessary treatments are seen as luxuries rather than rights, further entrenching health disparities. Adopting policies that facilitate equitable access could catalyze significant advancements in public health, ultimately benefiting everyone.
Additionally, studies are lacking on the impact of people from minority members of society. A lack of representation considering genetic, behavioral, and biochemical interactions compounds these issues. None of the practices that black and brown people participated in prior to colonization is considered. This includes the use of herbs, foods, and mental or spiritual practices. The only supported treatments within the conventional medical model rest on pharmaceuticals, surgery, or procedures if one is available. In this thinking, many preventable health concerns are dismissed because the patient, in essence, is not sick enough for conventional treatment. We are not used to waiting until something happens, but rather health was infused into our daily lives as Afro-Indigenous people.
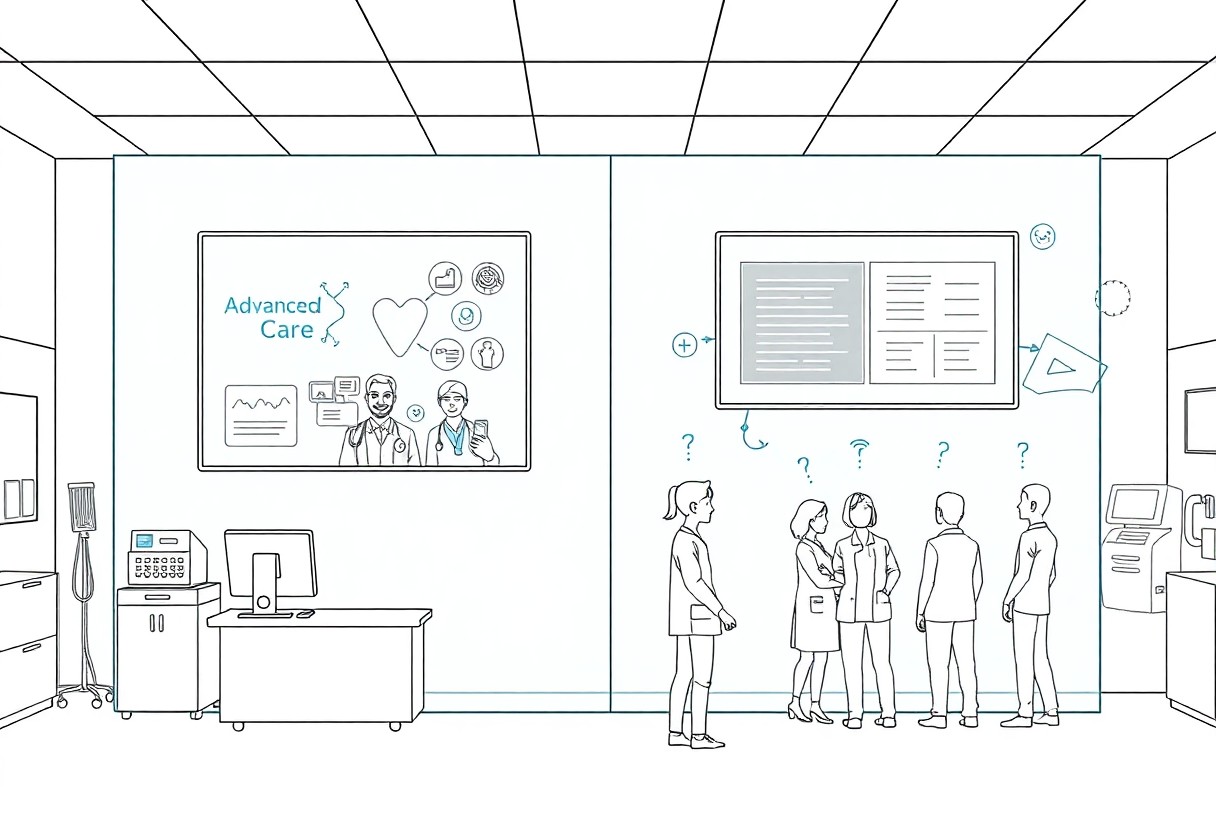
Digital Health Disparities: The New Frontier of Medical Apartheid
As healthcare increasingly shifts toward digital platforms, the disparities in access and utilization of technology reveal a troubling continuation of medical apartheid. Communities with limited internet access or insufficient technological literacy face significant barriers to care, impacting their health outcomes and exacerbating existing inequalities. This digital divide not only hinders individual access to information but also restricts participation in telemedicine, electronic health records, and health apps, leaving certain groups behind in an era where technology should serve as a great equalizer.
Technology Access and Its Implications for Care
Lack of access to reliable technology directly translates to diminished healthcare opportunities. With an estimated 22% of American households lacking broadband access, individuals in these environments cannot engage with necessary telehealth services. This disparity not only limits your ability to connect with healthcare providers but can also result in delayed diagnoses and treatments, worsening overall health outcomes and perpetuating the cycle of inequity in medicine.
Telehealth and the Risk of Exacerbating Existing Inequities
Telehealth holds promise for increasing access to care, yet it can unintentionally widen the gap between affluent and marginalized communities. If you lack a stable internet connection or digital literacy, telehealth services designed for convenience become inaccessible. In fact, studies show that lower-income populations are half as likely to use telehealth compared to their higher-income counterparts. This technological gap can result in poorer health management for those already facing significant barriers, leaving them to navigate complex health issues without adequate support.
While telehealth presents opportunities for many, it also poses serious risks of deepening existing inequities. For instance, if you belong to a low-income household with limited internet access, opportunities for virtual consultations or follow-ups may be entirely out of reach. Furthermore, disparities in health literacy can mean that even when services are available, they aren’t utilized effectively. As a result, the most vulnerable populations may find themselves further marginalized, unable to benefit from advancements that could otherwise improve their healthcare experiences and outcomes.
Advocacy and Reform: Building a More Equitable Healthcare System
Transforming the healthcare system requires a multifaceted approach that prioritizes equity and inclusivity. Advocates push for transparency in medical practices and equitable access to resources while demanding accountability from policymakers. By actively engaging communities and stakeholders, these efforts can address historical injustices and create sustainable change. The involvement of diverse voices is key in reshaping policies that currently marginalize vulnerable populations.
Grassroots Movements and Community Organizing
Grassroots movements play a pivotal role in advocating for healthcare equity, harnessing the power of community organizing to amplify voices often ignored by the system. Local activists mobilize residents to demand better access to medical resources and equitable treatment, using campaigns that educate and empower. Through efforts such as town halls and protest initiatives, marginalized communities unite to confront disparities and advocate for systemic reform.
Policy Changes and Their Potential for Long-Term Impact
Effective policy changes can reshape the healthcare landscape, particularly those that target systemic inequities. Initiatives like expanded Medicaid, funding for community health centers, and regulations against discriminatory practices can significantly improve health outcomes for marginalized groups. With the right policies in place, we can reduce disparities and enhance access to care, fostering a healthcare system that serves everyone equitably.
Specific policies have demonstrated significant potential for long-term impact. For example, states that have expanded Medicaid under the Affordable Care Act saw a 25% decrease in uninsured rates among low-income populations. Additionally, funding for community health organizations has been shown to decrease health disparities by addressing social determinants such as housing and education. By implementing comprehensive reforms that prioritize equity, we can create a sustainable framework that not only addresses immediate healthcare needs but also dismantles the systemic barriers that have long plagued our healthcare system.
Conclusion
From above, it is clear that medical apartheid is not just a chapter in our past; it permeates our present. I urge you to recognize the ongoing disparities and injustices within healthcare systems. You have the power to advocate for equitable treatment and challenge the status quo. Your awareness and actions can foster change, ensuring that all individuals receive the quality care they deserve, irrespective of their background. Let us not turn a blind eye to this critical issue but rather work collectively to dismantle the barriers that persist in healthcare today.
