2025 is set to be a transformative year for any functional medicine practitioner, as demand for holistic, patient-centered care reaches record highs. With the functional medicine market experiencing a 20% annual growth rate, countless practitioners are redefining what modern healthcare looks like. This guide is designed to empower both aspiring and experienced functional medicine practitioners with a clear, actionable roadmap to excel in this rapidly evolving landscape.
You will discover the foundational principles of functional medicine, step-by-step credentialing pathways, essential clinical and business skills, strategies for technology integration, and the trends shaping the future. Expect inspiring success stories, proven insights, and the direction you need to build a thriving practice in the new era of healthcare.
Understanding Functional Medicine in 2025
Functional medicine is transforming healthcare as more patients and clinicians seek holistic, personalized solutions. As a functional medicine practitioner, understanding the field's evolution in 2025 is vital for success. From new patient demographics to regulatory shifts, the landscape is dynamic and full of opportunity.
Defining Functional Medicine
At its core, functional medicine is based on root-cause analysis, systems biology, and patient-centered care. Unlike conventional medicine, which often addresses symptoms, the functional medicine practitioner focuses on prevention and personalized treatment.
| Functional Medicine | Conventional Medicine |
|---|---|
| Root-cause focus | Symptom management |
| Systems biology | Organ-specific |
| Personalized plans | Standard protocols |
For example, a functional medicine practitioner may help a patient reverse chronic disease through lifestyle changes rather than medication alone. The market is expanding rapidly, with a 20% annual growth rate reported by the Functional Medicine Market Growth Statistics.
Why Functional Medicine is Gaining Momentum
The surge in chronic illnesses and growing patient dissatisfaction with traditional care models are driving more people to functional medicine. The functional medicine practitioner is uniquely positioned to address these concerns by integrating lifestyle medicine and root-cause approaches.
Success stories abound, such as patients achieving autoimmune disease remission or improved metabolic health. Public awareness is rising, and 60% of patients now seek integrative care options, making this an opportune time for functional medicine practitioners to expand their impact.
The Evolving Patient Demographic
In 2025, the typical patient seeking a functional medicine practitioner is younger, tech-savvy, and highly health-literate. These patients value convenience and often prefer virtual or hybrid care models that fit their busy lifestyles.
Millennials, for example, are prioritizing preventive health and are quick to adopt digital health tools. As a functional medicine practitioner, adapting to these preferences is essential for meeting patient expectations and remaining competitive in the evolving healthcare environment.
Regulatory and Industry Shifts
Regulatory frameworks for functional medicine practitioners are evolving rapidly. Updates in licensure, certification, and insurance reimbursement are creating new opportunities and challenges. Major health systems are increasingly recognizing the value of functional medicine, as seen in the Cleveland Clinic Center for Functional Medicine's recent expansion.
Staying informed about these changes enables the functional medicine practitioner to maximize insurance billing and maintain compliance. This shifting landscape signals growing institutional support and professional legitimacy for the field.
Key Challenges and Opportunities
While the growth of functional medicine is promising, challenges remain. Navigating regulatory ambiguity and balancing scientific rigor with holistic care can be complex for any functional medicine practitioner.
Key opportunities include:
- Filling care gaps in underserved communities
- Integrating evidence-based approaches with holistic modalities
- Expanding access through virtual care
By addressing these challenges and leveraging opportunities, the functional medicine practitioner can play a pivotal role in shaping the future of healthcare.
Becoming a Functional Medicine Practitioner: Education, Training & Certification
Embarking on the journey to become a functional medicine practitioner in 2025 requires a clear understanding of modern educational pathways, credentialing processes, and the evolving landscape of integrative health. Whether you are a seasoned clinician or just starting, the right foundation ensures success in this dynamic field.
Educational Pathways
The path to becoming a functional medicine practitioner starts with a recognized health professional degree. Physicians (MD, DO), naturopathic doctors (ND), nurse practitioners (NP), chiropractors (DC), and physician assistants (PA) most commonly pursue this route.
For those from allied health backgrounds, such as registered dietitians or health coaches, specialized programs offer alternative entry points. Leading organizations like the Institute for Functional Medicine (IFM) and the American Academy of Anti-Aging Medicine (A4M) provide structured curricula.
Table: Common Entry Points
| Background | Entry Path |
|---|---|
| MD, DO, ND, NP, DC | Direct certification route |
| Health Coach, RD | Bridge or foundational track |
Selecting the right pathway is the first step for any aspiring functional medicine practitioner.
Certification and Credentialing
Certification validates your expertise as a functional medicine practitioner. The most recognized credential is the IFM Certified Practitioner (IFMCP), which requires completion of core modules, case studies, and a rigorous exam. Other bodies, such as the National Board for Health and Wellness Coaching (NBHWC), offer complementary certifications.
The process typically includes:
- Core coursework
- Clinical case submission
- Written and practical exams
Ongoing renewal and continuing education are essential to maintain certification and stay current. For a deeper understanding of market expectations and the value of credentialing, review the Functional Medicine Diagnostic Market Report.
Building Clinical Competence
To excel as a functional medicine practitioner, clinical competence is paramount. Core subjects include nutrition, genomics, toxicology, gut health, and mind-body medicine. Leading programs blend theory with practical experience.
Key training approaches:
- Case-based learning
- Mentorship with experienced clinicians
- Clinical immersion practicums
This hands-on exposure ensures that every functional medicine practitioner can confidently address complex patient needs.
Integrative and Holistic Skillsets
Modern patients seek a functional medicine practitioner with a broad, integrative skillset. Competence now means blending nutrition, herbal medicine, coaching, and mind-body techniques.
Equally important is a trauma-informed and culturally sensitive approach. For example, a practitioner managing a complex autoimmune case may coordinate nutrition, herbal support, and psychological counseling, tailoring care to individual backgrounds.
This holistic mindset empowers every functional medicine practitioner to deliver truly patient-centered care.
Navigating the Credentialing Landscape
The credentialing landscape for a functional medicine practitioner continues to evolve. In 2025, many states have updated licensure frameworks to accommodate integrative care. Insurance billing options are expanding, with a reported 15% increase in covered visits for functional medicine services last year.
Keep these essentials in mind:
- Check state and national licensure requirements frequently.
- Stay informed about insurance coding for functional medicine practitioner services.
- Leverage professional associations for up-to-date advocacy and support.
By navigating these requirements, each functional medicine practitioner is better equipped to build a sustainable, compliant practice.
Building a Thriving Functional Medicine Practice: Step-by-Step Roadmap
Launching a successful functional medicine practitioner career in 2025 requires a methodical and future-focused approach. This roadmap guides you through each essential step, from identifying your unique space in the market to measuring your ongoing impact. Here’s how to build a thriving, sustainable practice in the evolving healthcare landscape.
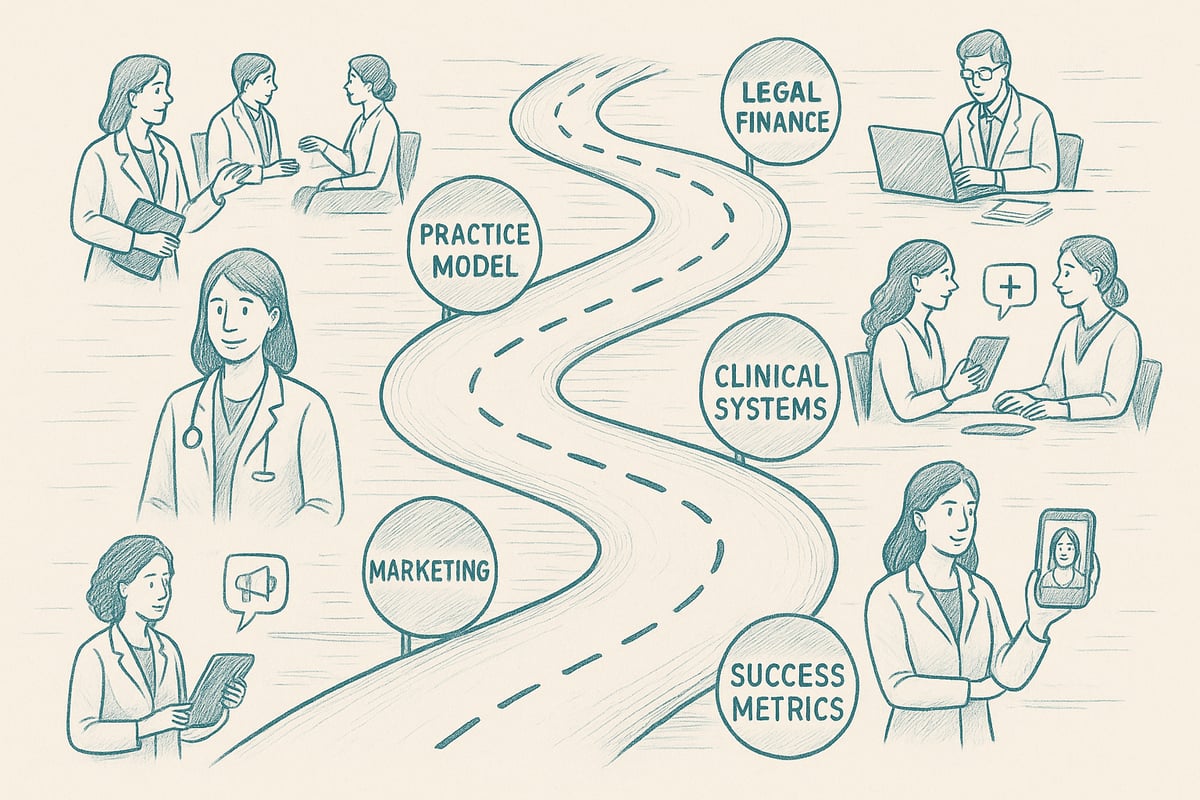
Step 1: Defining Your Niche and Ideal Patient
Every functional medicine practitioner begins by clarifying their unique value. Start by identifying underserved populations or focus areas, such as gut health, autoimmune conditions, or pediatric care. Assess your community’s needs and research which health concerns are most prevalent.
Specializing allows you to tailor your services and messaging, making it easier to stand out. For example, a functional medicine practitioner focusing on nutrition can capitalize on the growing health and wellness food market, which is expected to surge in coming years. This step lays the foundation for a meaningful and profitable practice.
Step 2: Designing Your Practice Model
Choosing the right practice model is critical for a functional medicine practitioner’s success. Options include solo practices, group collaborations, virtual care, hybrid setups, or membership-based models. Each structure offers different benefits and challenges regarding scalability, flexibility, and patient engagement.
A virtual-first model, for instance, appeals to tech-savvy patients and can reduce overhead costs. Evaluate your strengths, resources, and target market before deciding. The right model supports your vision and aligns with your patients’ preferences, helping you deliver care more efficiently.
Step 3: Setting Up Legal, Financial, and Operational Foundations
Establishing solid legal and financial foundations protects your functional medicine practitioner business. Select the appropriate business entity, such as LLC or corporation, and secure liability insurance. Ensure compliance with state and federal regulations to avoid costly setbacks.
Develop a financial plan that addresses startup costs, revenue streams, and pricing strategies. On average, opening a functional medicine clinic requires an investment between $50,000 and $150,000. Thorough planning early on ensures your practice remains sustainable and resilient.
Step 4: Clinical Systems and Patient Experience
Delivering exceptional care as a functional medicine practitioner depends on robust clinical systems. Streamline intake, assessment, and personalized care planning to optimize outcomes. Implement patient education initiatives, group visits, or health workshops to foster engagement and retention.
Consider how you’ll manage follow-ups, collect feedback, and adjust plans based on data. Prioritizing a seamless patient journey not only boosts satisfaction but also encourages referrals and long-term loyalty.
Step 5: Marketing and Patient Acquisition
Building a strong online presence is essential for a functional medicine practitioner in 2025. Develop a professional website, invest in SEO, and maintain active social media profiles. These channels help you connect with prospective patients and share your expertise.
Community outreach, referral networks, and local partnerships further expand your reach. According to a 2023 survey, 70 percent of new patients find their practitioners online. A strategic marketing plan ensures a steady flow of new clients and supports your growth goals.
Step 6: Leveraging Technology and Digital Tools
Integrating technology is now non-negotiable for any functional medicine practitioner aiming to stay competitive. Use electronic health records, telemedicine platforms, and patient portals to streamline communication and care delivery.
Remote monitoring tools and apps can enhance nutrition tracking and progress monitoring for your patients. Choose HIPAA-compliant solutions that protect sensitive data while improving efficiency. Technology not only simplifies operations but also elevates the patient experience.
Step 7: Measuring Success and Continuous Improvement
A thriving functional medicine practitioner consistently measures and improves performance. Track key indicators such as patient outcomes, retention rates, and revenue to assess progress. Use quality improvement cycles to refine your clinical and business processes.
Collect patient satisfaction surveys to gain actionable insights and identify areas for growth. Commit to ongoing education and innovation so your practice remains relevant and effective in the rapidly evolving healthcare environment.
Essential Skills and Mindsets for Success in 2025
Thriving as a functional medicine practitioner in 2025 requires more than clinical expertise. Success hinges on a mindset of lifelong growth, strong communication, business savvy, and a commitment to personal well-being. Let’s explore the skillsets that set leaders apart in this dynamic field.
Clinical Excellence and Lifelong Learning
A functional medicine practitioner must stay ahead of evolving science and best practices. Engaging with the latest research, attending annual conferences, and participating in webinars are vital for continuous improvement.
For example, the annual IFM conference delivers deep dives into emerging topics and offers networking with thought leaders. Peer review and case discussions also foster professional growth.
Investing in ongoing education ensures that a functional medicine practitioner provides the highest standard of care. This commitment builds patient trust and supports evidence-based practice.
Communication and Coaching Skills
Strong communication sets a functional medicine practitioner apart. Skills like motivational interviewing and health coaching empower patients to take charge of their health.
Building therapeutic alliances through shared decision-making leads to better outcomes. In fact, patients with strong relationships with their functional medicine practitioner demonstrate 30 percent higher adherence to treatment plans.
Mastering these tools not only improves patient satisfaction, it also creates lasting partnerships on the path to wellness.
Business Acumen and Leadership
Running a successful practice means mastering business fundamentals. A functional medicine practitioner should understand financial management, team leadership, and efficient operations.
Implementing standard operating procedures (SOPs) helps streamline daily tasks and delegate responsibilities. Staying informed about industry trends, such as those highlighted in the Natural Health Products Market Forecast, enables practitioners to anticipate shifts that may impact their services.
Leadership is about creating a positive culture, supporting staff development, and positioning your functional medicine practitioner business for sustainable growth.
Resilience and Self-Care
The demands of being a functional medicine practitioner make self-care essential. Mindfulness practices, clear boundaries, and work-life balance protect against burnout.
Engaging in peer support and supervision provides a safe space to process challenges. Adopting evidence-based self-care protocols has led to a 40 percent improvement in practitioner well-being.
A resilient functional medicine practitioner models healthy behaviors for patients and sustains their passion for transformative care.
Integrating Advanced Tools and Technologies in Functional Medicine
In 2025, advanced tools and digital innovations are rapidly transforming the way a functional medicine practitioner delivers care. Leveraging these technologies not only enhances patient outcomes but also streamlines workflows and expands access to personalized medicine.
Digital Health Platforms and Telemedicine
The adoption of digital health platforms has become essential for the functional medicine practitioner. Secure telemedicine tools now support remote consultations and ongoing patient monitoring, making care accessible beyond traditional office walls.
These platforms offer:
- HIPAA-compliant video visits
- Integrated electronic health records (EHR)
- Secure messaging and document sharing
In 2024, telehealth adoption grew by 38% as more patients sought convenient, tech-enabled care. A functional medicine practitioner can now monitor patient progress in real time, adjust treatment plans remotely, and maintain strong patient relationships regardless of location.
Personalized Medicine: Genomics and Biomarkers
Personalized medicine is at the forefront for every functional medicine practitioner in 2025. Genetic testing and advanced biomarker analysis enable practitioners to tailor interventions based on each patient’s unique biology.
Key applications include:
- Nutrigenomics for individualized nutrition plans
- Early detection of disease risk
- Customized supplement and lifestyle recommendations
Ethical considerations and proper interpretation of results are critical. For those seeking rigorous training, organizations like the Institute for Functional Medicine offer comprehensive education on genomics integration. By embracing these tools, a functional medicine practitioner can deliver more precise, impactful care.
Artificial Intelligence and Decision Support
Artificial intelligence is empowering the functional medicine practitioner with new decision support capabilities. AI-powered tools analyze complex datasets, suggest risk stratification, and optimize clinical protocols.
Benefits include:
- Automated patient intake triage
- Data-driven treatment recommendations
- Enhanced identification of patterns in chronic disease
A functional medicine practitioner can use AI to streamline intake, reduce administrative burden, and stay current with the latest evidence. As AI technology evolves, its role in supporting clinical judgment and improving patient outcomes will only expand.
Wearables and Patient Engagement Tools
Wearable technology is revolutionizing how a functional medicine practitioner engages patients in their own health journey. Devices such as fitness trackers, sleep monitors, and smart health apps generate real-time data that inform personalized care.
Common tools include:
- Activity and heart rate monitors
- Continuous glucose monitors
- Mobile health applications
According to a 2024 survey, 65% of patients now use at least one wearable device. By integrating this data, a functional medicine practitioner can create actionable recommendations, boost patient accountability, and track progress with greater accuracy.
The Future of Functional Medicine: Trends, Opportunities, and Challenges
As the healthcare landscape transforms, the future for every functional medicine practitioner shines with possibility. Emerging trends, evolving policies, and new technologies are reshaping how practitioners deliver care, collaborate, and grow their practices. Understanding these shifts is crucial for long-term success.
Expanding Access and Health Equity
The modern functional medicine practitioner is positioned to bridge gaps in healthcare access. Telehealth and mobile clinics are making holistic care more available to rural and underserved communities. Programs that deliver functional medicine in federally qualified health centers are breaking down barriers for marginalized groups.
Key initiatives include:
- Community health partnerships
- Sliding scale or flexible payment options
- Multilingual patient education resources
By prioritizing health equity, the functional medicine practitioner is not only improving individual outcomes but also uplifting entire communities.
Collaborative Care and Interdisciplinary Teams
A functional medicine practitioner thrives in collaborative environments. Working alongside conventional physicians, health coaches, and specialists, they build interdisciplinary teams that deliver seamless, patient-centered care. This team approach is especially valuable for managing complex, chronic conditions.
Benefits of interdisciplinary care:
- Diverse perspectives for comprehensive treatment plans
- Improved patient adherence and satisfaction
- 25% better outcomes, as reported by the BMJ in 2023
For the functional medicine practitioner, embracing collaboration is essential to driving exceptional results and broadening their scope of impact.
Policy, Insurance, and Advocacy
Changing policies are shaping how every functional medicine practitioner operates. Recent legislative advances and insurance updates are increasing reimbursement for integrative services. Some states now mandate coverage for certain functional medicine interventions, expanding patient access.
Effective advocacy efforts include:
- Staying informed on licensure and reimbursement updates
- Participating in professional advocacy groups
- Educating policymakers about the value of integrative care
By engaging in advocacy, the functional medicine practitioner helps shape a more supportive regulatory environment for holistic medicine.
Lifelong Growth and Professional Networks
Continuous growth is a hallmark of a successful functional medicine practitioner. Building strong professional networks, seeking mentorship, and joining organizations such as the Institute for Functional Medicine can double practice growth rates.
Ways to foster ongoing development:
- Attending conferences and workshops
- Participating in peer supervision groups
- Sharing case studies and best practices
For every functional medicine practitioner, investing in professional relationships and lifelong learning ensures adaptability and resilience in a rapidly changing field.
As you look ahead to building a thriving, future-ready practice, remember that ongoing learning and community support are essential. The strategies we covered—from mastering clinical skills to embracing the latest health tech—are just the beginning. If you’re ready to deepen your understanding and take the next step on your journey, I invite you to explore our free foundational course, where you’ll connect with like-minded practitioners and gain practical insights you can use right away. Start your path to empowered, holistic care with Intro to Holistic Medicine I.
