
Most people enter the medical field with a mission to help others, driven by a desire to heal and support patients. However, as I examined deeper into healthcare at an early age, I recognized the potential dangers associated with certain practices and the unintended consequences they can have on individuals’ lives. This realization prompted me to take a step back and reassess my approach and consideration to healing, prioritizing patient well-being above all. In this post, I will share my journey toward standing for a holistic perspective on care and how it led me to make a transformative choice for both myself and my patients.
Key Takeaways:
- Challenges the traditional medical model and advocates for alternative approaches to health.
- Emphasizes the importance of patient-centered care and informed consent.
- Highlights personal experiences and reflections that led to a re-evaluation of medical practices.
The Ethical Dilemma: Harm vs. Healing
The ethical conflict between inflicting harm and promoting healing is at the core of medical practice. I often found myself grappling with the troubling reality that many established treatments resulted in significant side effects, ultimately causing more distress for patients than their illnesses. The stories and the cases I have heard I cannot unhear. I have commonly referred to myself as the clean up crew of medicine weeding through medical neglect, gaslighting, errors, runarounds, and medical trauma. This conflict prompted my exploration of “First do no harm”: Medical School Admissions Requirements …, pushing me to question whether the traditional path truly aligned with my commitment to patient welfare. As a young girl, I always knew I would be a doctor but watched up close and personal the failures of conventional medical treatments in healing, but the strengths in managing diseases.
The Flaws in Conventional Medical Practices
Conventional medical practices often prioritize protocols over individual patient needs. Frequently, I observed that standardized treatments led to a one-size-fits-all approach, sometimes disregarding patients’ unique circumstances and comprehensive well-being. The reliance on pharmaceuticals, rather than holistic assessments, raised concerns about potential adverse effects that could exacerbate underlying issues rather than resolve them. I realized that while technology advances, it often overshadows the human element of care, leaving patients feeling sidelined. Many patients are often unheard, dismissed, or even experience adversarial relationships with doctors. I often hear statements like, “I do not trust doctors,” or “I do not go to doctors,” as well as from patients who are hesitant to be open with their doctor due to fear of being judged or misunderstood.
Examining the Oath: What “First, Do No Harm” Really Means
Interpreting the Hippocratic Oath revealed profound insights about ethical medical practice. I questioned whether adhering strictly to this ancient principle felt authentic in an environment increasingly motivated by profit rather than patient-centered care. The concept of “first, do no harm” is not merely about avoiding physical pain; it extends to the emotional and psychological impact of medical decisions. Aligning this oath with my values required a deeper understanding of care beyond conventional methods, leading me to advocate for alternatives that genuinely consider the patient’s whole being.
The definition of “do no harm” is more complex than often assumed. Examining the intricacies of medical practice highlighted a disconnection between the oath’s intent and its execution. For instance, treatments may relieve symptoms but simultaneously neglect the root causes of discomfort, resulting in increased long-term issues for the patient. I began to see how unnecessary interventions can catalyze harm, reinforcing my belief that ethical alternatives could provide more sustainable healing. Fostering an approach that deeply honors the oath demands not just awareness of physical interventions, but a commitment to overall well-being, paving the way for truly meaningful healthcare practices.
The Quest for Alternatives: Exploring Holistic Approaches
In my upbringing it was a blessing to have been led to many alternative treatments. These “alternative treatments” were connected to indigenous practices, or practices that came from the spirit, not science. In my education, I chose education that led me to explore holistic approaches that treat the body as an interconnected whole rather than isolated symptoms. These methods emphasize the importance of lifestyle, environment, and emotional well-being, highlighting that physical ailments often stem from deeper-rooted issues. I discovered that integrating various healing practices can complement conventional medicine, offering a more balanced path to wellness that resonates with those yearning to feel empowered in their health journey. Conventional medicine is not the enemy, but it is not always the solution either.
Integrative Medicine: Blending Science and Wholeness
Integrative medicine combines conventional treatments with holistic practices, fostering a comprehensive approach to health. I found that it embraces evidence-based practices, such as nutrition, acupuncture, and mindfulness, enhancing overall wellness. This integration allows individuals to benefit from the best of both worlds, empowering you to take an active role in your healing process while addressing not only physical symptoms but also emotional and spiritual components.
Personal Case Study: Transformative Experiences with Natural Remedies
My journey includes transformative experiences with natural healing that shifted my perspective on health. Having experienced the impacts of intergenerational trauma and my desire to stop the cycle, I focused on healing and balancing my own physical, environmental, mental, emotional, spiritual, and ancestral health. The complexity of food plans, supplement choices, herbal remedies, energy work, biofeedback, neurofeedback, meditation, yoga, and hundreds of other modalities.
Conventional medicine only offered limited solutions to treat my complex trauma and various responses mentally, emotionally, and behaviorally associated with complex trauma compounded by intergenerational trauma. I followed my intuition, which led and guided me to healers, teachers, programs, schools, food, meditation, breathwork, and more. My personal journey of healing, along with assisting others in their healing process, has led me to reflect on the patterns of healing.
By following the therapeutic order, I have transcended the “this is your only option ” learning, first-hand, how a person can heal themselves if they are at the center of their own healing. The holistic framework has a rhythm in practice and is one that I have led thousands of others to unlock with them. These experiences not only validated my decision to explore alternatives but also ignited a passion for sharing these methods with others seeking similar relief.
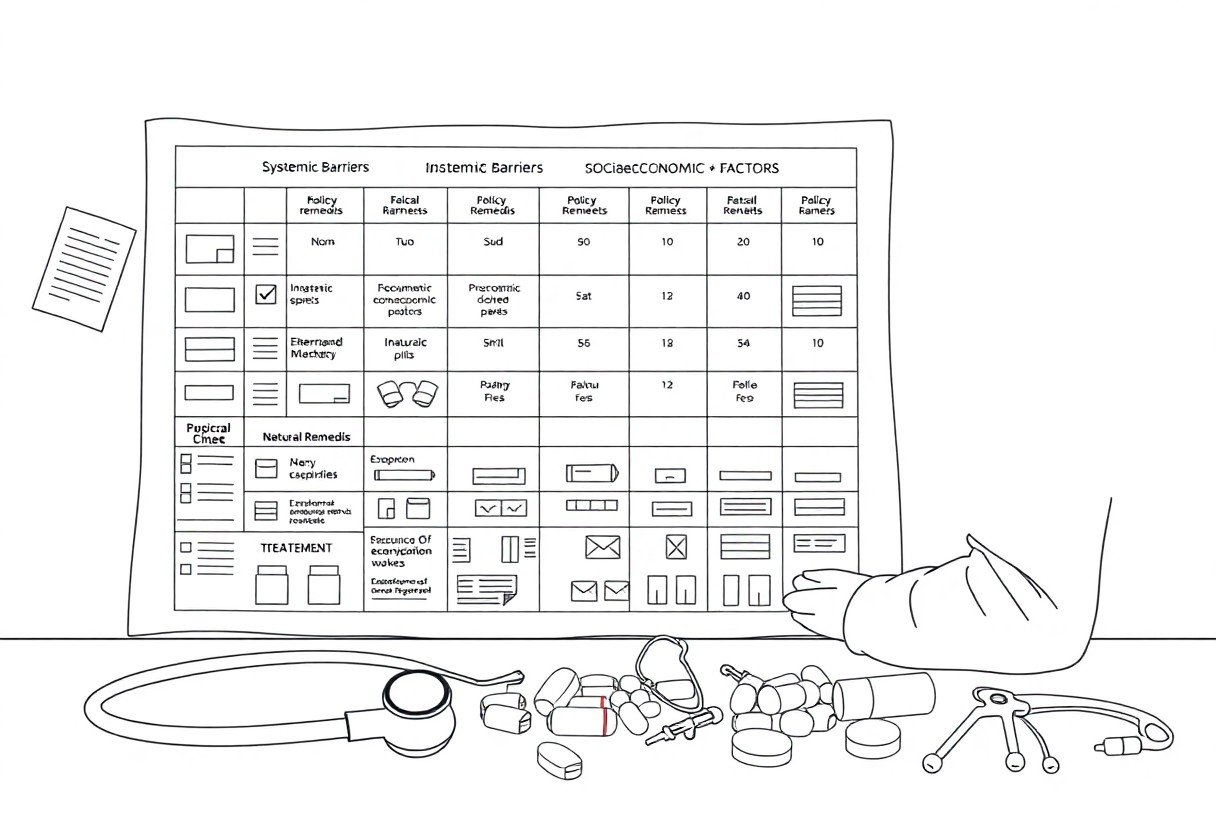
The Impact of Systemic Issues on Healthcare Choices
Systemic issues within healthcare profoundly shape the decisions patients and providers make. Factors like economic disparities, vague pricing structures, and information asymmetry create barriers that limit informed choices. These challenges often push individuals toward solutions that may not be in their best interest, while the broader healthcare system prioritizes profit over patient well-being. The interconnectedness of these systemic problems can lead to a misalignment between patient needs and available care options, making it vital to address these root causes for genuine progress.
Understanding the Influence of Pharmaceutical Industries
The pharmaceutical industry exerts significant influence over healthcare choices through aggressive marketing tactics and strategic lobbying. I’ve witnessed how this can skew the perception of necessity and efficacy of treatments. Often, drugs are promoted as the first solution rather than lifestyle adjustments or alternative treatments. This prioritization shapes doctors’ prescribing habits and ultimately affects patient expectations, leading to a cycle where the reliance on pharmaceuticals overshadows other viable options.
The Role of Insurance: Accessibility and Affordability
Insurance dictates the accessibility and affordability of healthcare, impacting every individual’s ability to access necessary treatments. Coverage disparities often force patients to navigate a complex web of policies that can limit options and drive up out-of-pocket expenses. The system frequently incentivizes treatment protocols that may not align with holistic care, pushing you toward practices that may not be the most beneficial for your health.
Insurance plans often dictate which treatments and medications are covered, leaving patients with high out-of-pocket costs for crucial care. For instance, only 30% of individuals with chronic conditions find their needs fully met by standard insurance coverage. Out-of-network providers may offer a wider range of holistic options; however, over 60% of patients report confusion about insurance benefits, effectively sidelining alternative solutions. Navigating these barriers requires you to be proactive in understanding your plan and advocating for the care that best suits your needs.
The Power of Empowerment: Educating Patients for Better Choices
Empowerment begins with knowledge. By providing patients with adequate information about their conditions and treatment options, they can actively participate in their healthcare decisions. This process encourages individuals to ask questions, seek second opinions, and choose alternatives that align with their values. Medical professionals who prioritize education create a foundation for partnership, leading to personalized care that genuinely addresses patient needs.
Educating patients fosters a sense of ownership over their health journeys. For instance, programs that teach self-management techniques have proven effective in chronic conditions, with studies showing a reduction in hospital admissions by up to 30%. When you understand your options and potential risks, you can weigh them against your personal beliefs and lifestyle. Knowledge equips you to engage with healthcare providers meaningfully, ultimately reorienting the dynamic from passive receiver to active participant. This shift not only improves health outcomes but also enhances overall satisfaction with the care received.
Advocacy for Change: Steps Toward a Safer Healthcare System
Advocacy for change within our healthcare system requires a multi-faceted approach that addresses the root causes of harm. I believe in rallying stakeholders across various sectors to push for policies prioritizing patient safety, transparency, and ethical practices. Establishing forums for dialogue between practitioners and patients can shine a light on systemic issues while fostering collaborative solutions. Through education and awareness, we can create an environment where patient-centric care becomes the norm rather than the exception.
Strategies for Practitioners to Adopt Ethical Practices
Practitioners can implement various strategies to enhance ethical practices within their care environments. Adopting a culture of open communication is vital; it allows patients to express concerns and contributes to shared decision-making. Continuous professional development, focusing on ethical dilemmas and case studies, equips providers to make informed choices that prioritize patient well-being. Additionally, incorporating regular feedback mechanisms can help identify areas for improvement, ensuring that ethical standards remain at the forefront of healthcare delivery.
Mobilizing Public Opinion: How to Encourage System Reform
Mobilizing public opinion is necessary for creating momentum around healthcare reform. Engaging communities through awareness campaigns and social media can increase visibility for systemic issues that impact patient safety. Utilizing storytelling to share real-life experiences allows individuals to connect emotionally, fostering a sense of urgency for change. Partnering with advocacy groups can amplify these efforts, creating a unified voice demanding accountability and reform.
Enhancing public awareness about healthcare challenges requires a concerted effort to shift perceptions. Highlighting statistics, such as the medical error rate contributing to approximately 250,000 deaths annually in the U.S., illustrates the gravity of the situation. Utilizing testimonials from patients affected by systemic failures can personalize these statistics and galvanize support. Hosting community forums and workshops offers an interactive platform for dialogue, arming citizens with knowledge to advocate for their rights effectively. Additionally, leveraging traditional and digital media amplifies messages, ensuring a broader reach and fostering a collective push for necessary reforms.
Summing up
So, I chose a different path in my healthcare education journey because I believe in the principle of “First, Do No Harm.” My decision was driven by the desire to prioritize patient safety and well-being above all else. By exploring alternative practices and treatment methodologies, I aim to enhance understanding and foster a more compassionate approach to healthcare. I encourage you to consider the implications of your choices and recognize the profound impact they can have on the lives of those you serve.
If you want to learn about how to practice a holistic lifestyle, grab your free starter guide
